Silent Suffering: Recognizing and Addressing the Emotional Impact of Patient Loss on Medical Students
DOI:
https://doi.org/10.5195/ijms.2024.2689Keywords:
Medical Education, Patient loss, Resilience, wellbeing, Coping Strategies , Healthcare Providers, Reflection , Emotional Responses, Burnout , Supportive Environment, Palliative Care , Student Wellness, Professionalism , End-of-life Care, Vulnerability , Mental Well-being, Sadness , Guilt, Debriefing Sessions , Clinical RotationsAbstract
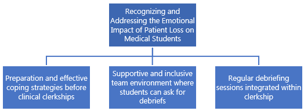
Experiencing patient loss is emotionally challenging for many medical students. This narrative reflects on the author's encounter with sudden patient loss and the complex emotions it evoked. The commentary underscores the need to prioritize emotional support for medical students dealing with patient loss. The author proposes ways to accomplish this, including equipping students with effective coping mechanisms, creating a supportive environment that encourages students to seek debriefing sessions, and incorporating debriefing sessions into clerkship curricula. By normalizing the emotional complexities of patient loss and fostering a culture of support, medical education can better prepare students to navigate the challenges of patient care with compassion and resilience.
References
Pessagno R, Foote CE, Aponte R. Dealing with death: medical students' experiences with patient loss. Omega (Westport). 2013;68(3):207-28. DOI: https://doi.org/10.2190/OM.68.3.b
Rhodes-Kropf J, Carmody SS, Seltzer D, Redinbaugh E, Gadmer N, Block SD, Arnold RM. "This is just too awful; I just can't believe I experienced that...": medical students' reactions to their "most memorable" patient death. Acad Med. 2005;80(7):634-40. DOI: https://doi.org/10.1097/00001888-200507000-00005
Williams CM, Wilson CC, Olsen CH. Dying, death, and medical education: student voices. J Palliat Med. 2005;8(2):372-81. DOI: https://doi.org/10.1089/jpm.2005.8.372
Kelly E, Nisker J. Medical students’ first clinical experiences of death. Med Educ. 2010;44(4):421-8. DOI: https://doi.org/10.1111/j.1365-2923.2009.03603.x
Paul Richard W. The lived experience of physicians dealing with patient death. BMJ Support Palliat Care. 2014;4(3):271. DOI: https://doi.org/10.1136/bmjspcare-2012-000326
Sullivan AM, Lakoma MD, Block SD. The status of medical education in end-of-life care: a national report. J Gen Intern Med. 2003;18(9):685-95. DOI: https://doi.org/10.1046/j.1525-1497.2003.21215.x
Kaye JM, Loscalzo G. Learning to care for dying patients: a controlled longitudinal study of a death education course. J Cancer Educ. 1998;13(1):52-7.
Schallenburger M, Schwartz J, Batzler YN, Meier S, Küppers R, Tenge T, et al. Handling the desire to die- evaluation of an elective course for medical students. BMC Med Educ. 2024;24(1):279. DOI: https://doi.org/10.1186/s12909-024-05269-6
Klein HJ, McCarthy SM. Student wellness trends and interventions in medical education: a narrative review. Humanit Soc Sci Commun. 2022;9(1):92. DOI: https://doi.org/10.1057/s41599-022-01105-8
Ratanawongsa N, Teherani A, Hauer KE. Third-year medical students' experiences with dying patients during the internal medicine clerkship: a qualitative study of the informal curriculum. Acad Med. 2005;80(7):641-7. DOI: https://doi.org/10.1097/00001888-200507000-00006
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Grace Kim

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org







