A Cross-Sectional Institutional Survey of Depression, Suicidal Ideation, and Stigma in Medical Students
DOI:
https://doi.org/10.5195/ijms.2024.2664Keywords:
Humans Female Students, Depressive Disorder, Major Mentors Patient Health Questionnaire Schools, Medical Surveys and Questionnaires, Medical Depression Cross-Sectional Studies Suicidal Ideation Stereotyping Binge DrinkingAbstract
Background: Due to high rates of depression and suicidal ideation among medical students, interventions, such as Pass/Fail grading systems and peer-mentorship, have been implemented, but their effects not reported. The purpose of this study was to explore variations in depression severity among medical students and to better understand the related stigma in healthcare over the past decade, with the aim of enhancing medical education.
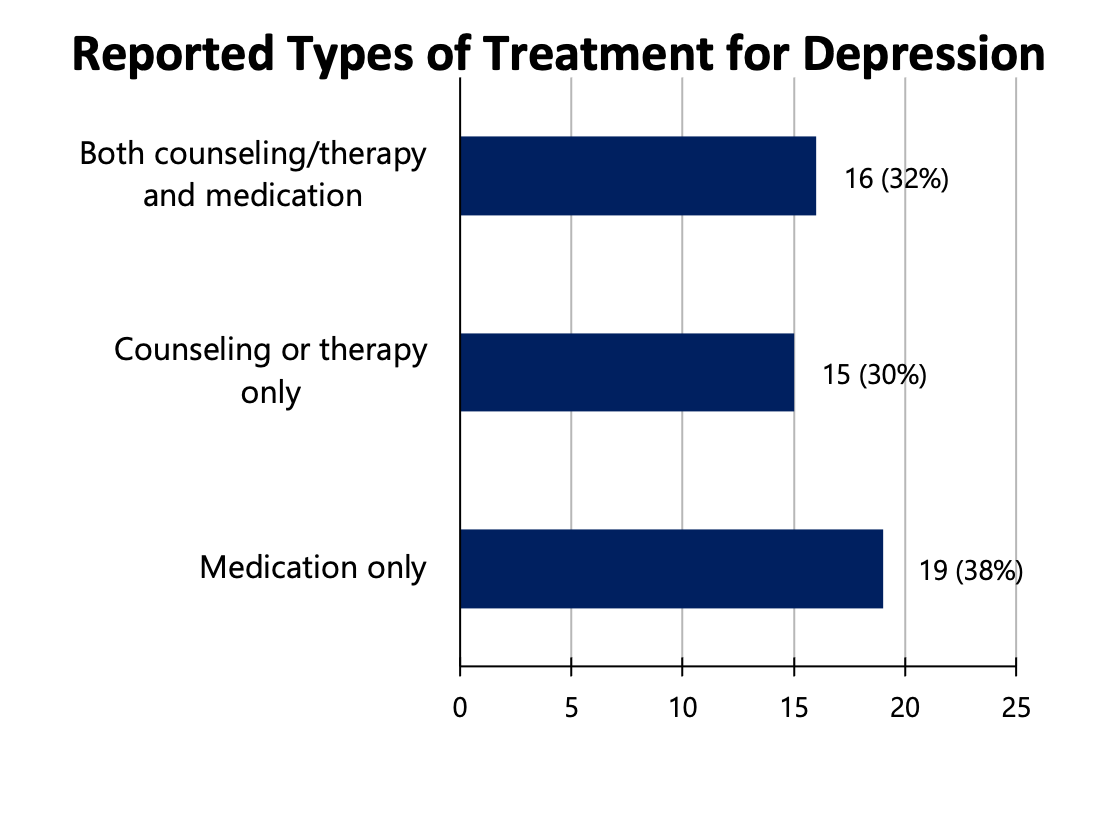
Methods: A cross-sectional survey was conducted on REDCap across students at the University of Illinois College of Medicine. The severity of depression was measured by the PHQ-9. Stigma was assessed utilizing Likert scale responses. Demographics of students who are most likely to experience depression were collected. Additionally, clinical diagnoses of depression, treatment modalities, and alcohol use were compared.
Results: There were 178 respondents with a 15% response rate. Thirty-nine (22%) respondents were classified in the moderate-to-severe depression group. Thirteen students, all female, endorsed suicidal ideation. A majority of respondents reported that depressed medical students would provide inferior patient care (n=71, 58%), their application to residency would be less competitive (n=76, 54%), they would feel embarrassed (n=88, 61%), and that it would be risky to reveal they have depression on a residency application (n=153, 94%).
Conclusions: Depression, suicidal ideation, and stigmatization remain prevalent in medical students and may have worsened since 2010. New, multi-faceted approaches such as giving medical students the choice of mental health providers, providing clear information about documentation, and implementing personal, well-being goals are needed to reduce depression and stigma experienced by medical students.
References
Bannatyne AJ, Jones C, Craig BM, Jones D, Forrest K. A systematic review of mental health interventions to reduce self-stigma in medical students and doctors. Front Med (Lausanne). 2023;10:1204274.
Dyrbye LN, Thomas MR, Power DV, Durning S, Moutier C, Massie FS Jr, et al. Burnout and serious thoughts of dropping out of medical school: a multi-institutional study. Acad Med. 2010;85(1):94-102.
Centers for Disease Control and Prevention. WISQARS (Web-based Injury Statistics Query and Reporting System). Available from: https://www.cdc.gov/injury/wisqars/index.html. Last updated Nov 8, 2023; cited Dec 5, 2023.
American Medical Association. Going directly from college to medical school: what it takes. Available from: https://www.ama-assn.org/medical-students/preparing-medical-school/going-directly-college-medical-school-what-it-takes. Last updated Aug 9, 2019; cited Dec 5, 2023.
Grow HM, McPhillips HA, Batra M. Understanding physician burnout. Curr Probl Pediatr Adolesc Health Care. 2019;49(11):100656.
Laitman BM, Muller D. Medical student deaths by suicide: the importance of transparency. Acad Med. 2019;94(4):466-8.
Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA. 2016;316(21):2214-36.
Hankir AK, Northall A, Zaman R. Stigma and mental health challenges in medical students. BMJ Case Rep. 2014;2014:bcr2014205226.
Cassano P, Fava M. Depression and public health: an overview. J Psychosom Res. 2002;53(4):849-57.
Klein HJ, McCarthy SM. Student wellness trends and interventions in medical education: a narrative review. Humanit Soc Sci Commun. 2022;9(1):1-8.
Snider CJ, Flaherty MP. Stigma and mental health: the curious case of COVID-19. Ment Health Glob Chall. 2020;3(1):27-32.
Schwenk TL, Davis L, Wimsatt LA. Depression, stigma, and suicidal ideation in medical students. JAMA. 2010;304(11):1181-90.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606-13.
Smarr KL, Keefer AL. Measures of depression and depressive symptoms: Beck Depression Inventory-II (BDI-II), Center for Epidemiologic Studies Depression Scale (CES-D), Geriatric Depression Scale (GDS), Hospital Anxiety and Depression Scale (HADS), and Patient Health Questionnaire-9 (PHQ-9). Arthritis Care Res (Hoboken). 2011;63 Suppl 11:S454-66.
Jebb AT, Ng V, Tay L. A review of key Likert scale development advances: 1995-2019. Front Psychol. 2021;12:637547.
Wechsler H, Dowdall GW, Davenport A, Rimm EB. A gender-specific measure of binge drinking among college students. Am J Public Health. 1995;85(7):982-5.
Goodwin RD, Dierker LC, Wu M, Galea S, Hoven CW, Weinberger AH. Trends in U.S. depression prevalence from 2015 to 2020: the widening treatment gap. Am J Prev Med. 2022;63(5):726-33.
Nair M, Moss N, Bashir A, Garate D, Thomas D, Fu S, et al. Mental health trends among medical students. Proc (Bayl Univ Med Cent). 2023;36(3):408-10.
West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283(6):516-29.
Cook AF, Arora VM, Rasinski KA, Curlin FA, Yoon JD. The prevalence of medical student mistreatment and its association with burnout. Acad Med. 2014;89(5):749-54.
Dyrbye L, Shanafelt T. A narrative review on burnout experienced by medical students and residents. Med Educ. 2016;50(1):132-49.
Snow PC, Harvey PJ, Cocking KL. Fitness-to-practice concerns in rural undergraduate medical education: a qualitative study. BMC Med Educ. 2014;14:195.
Corrigan P. How stigma interferes with mental health care. Am Psychol. 2004;59(7):614-25.
Suwalska J, Suwalska A, Szczygieł M, Łojko D. [Medical students and stigma of depression. Part 2. Self-stigma]. Psychiatr Pol. 2017;51(3):503-13. Polish.
Knaak S, Mantler E, Szeto A. Mental illness-related stigma in healthcare: barriers to access and care and evidence-based solutions. Healthc Manage Forum. 2017;30(2):111-6.
Tjia J, Givens JL, Shea JA. Factors associated with undertreatment of medical student depression. J Am Coll Health. 2005;53(5):219-24.
Seo C, Di Carlo C, Dong SX, Fournier K, Haykal KA. Risk factors for suicidal ideation and suicide attempt among medical students: a meta-analysis. PLoS One. 2021;16(12):e0261785.
Peng P, Hao Y, Liu Y, Chen S, Wang Y, Yang Q, et al. The prevalence and risk factors of mental problems in medical students during COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord. 2023;321:167-81.
Trostler M, Li Y, Plankey MW. Prevalence of binge drinking and associated co-factors among medical students in a U.S. Jesuit university. Am J Drug Alcohol Abuse. 2014;40(4):336-41.
Shah AA, Bazargan-Hejazi S, Lindstrom RW, Wolf KE. Prevalence of at-risk drinking among a national sample of medical students. Subst Abus. 2009;30(2):141-9.
Yoo HH, Cha SW, Lee SY. Patterns of alcohol consumption and drinking motives among Korean medical students. Med Sci Monit. 2020;26:e921613.
Tyssen R, Vaglum P, Aasland OG, Grønvold NT, Ekeberg O. Use of alcohol to cope with tension, and its relation to gender, years in medical school and hazardous drinking: a study of two nationwide Norwegian samples of medical students. Addiction. 1998;93(9):1341-9.
Moir F, Yielder J, Sanson J, Chen Y. Depression in medical students: current insights. Adv Med Educ Pract. 2018;9:323-33.
Ayala EE, Winseman JS, Johnsen RD, Mason HR. U.S. medical students who engage in self-care report less stress and higher quality of life. BMC Med Educ. 2018;18(1):189.
Waqas A, Malik S, Fida A, Abbas N, Mian N, Miryala S, et al. Interventions to reduce stigma related to mental illnesses in educational institutes: a systematic review. Psychiatr Q. 2020;91(3):887-903.
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Fiona Gruzmark, Alexis Reinders, Yanzhi Wang, Ryan Finkenbine

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org







