A Review of Psychosocial Factors on Birth Outcomes in Women with Substance Use Disorder in the United States: The Importance of Preventing Relapse During Sustained Remission
DOI:
https://doi.org/10.5195/ijms.2024.2166Keywords:
pregnancy, psychosocial factors, Relapse, Substance Use Disorders, Pregnancy Outcomes, Infant Mortality, Socioeconomic Factors, Mental Health, Stress, Psychological, Opioid-Related Disorders, Relapse Prevention, Prenatal Care, Social Stigma, Post-Traumatic Stress Disorder, Substance Abuse Treatment Centers, Cognitive Behavioral Therapy, Motivational Interviewing, Screening Tools, Pregnancy Complications, Healthcare Disparities, Preterm Birth, Neonatal Abstinence Syndrome, Maternal Health ServicesAbstract
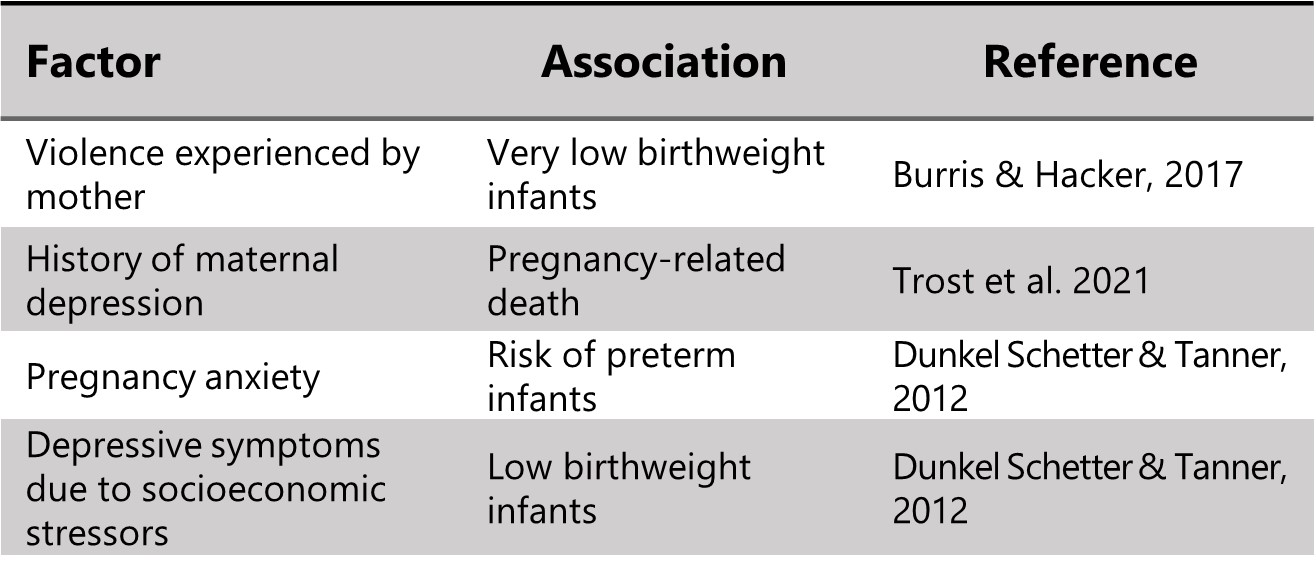
Infant mortality rate has been an area of concern for the United States for years. Many attributing factors, including psychosocial influences, have been identified. Pregnant patients with substance use disorder have also been shown to experience poor birth outcomes. This study examines trends related to socioeconomic hurdles and mental health in pregnant women with substance use disorder. Databases were searched to find resources that outlined these relationships. After assessing the study designs and associations of fifty-five resources, several patterns were observed, including an increased risk of adverse birth outcomes with higher maternal stress and lower socioeconomic status. In pregnant women with substance use disorder, post-traumatic stress and social stigma resulted in negative effects on mental health. Substance use-related pregnancy anxiety was amplified by triggers that resulted in feelings of fetal detachment and substance cravings. Most literature focused on pregnant patients with active addiction; however, these triggers may have an especially powerful effect on women who become pregnant while in substance use recovery. Studies on remission trajectories indicated a higher mortality risk in people with a history of substance use but have not yet calculated the proportion of women capable of bearing children in this category. This highlights the necessity to develop personalized treatment for pregnant women in sustained remission from substance use disorder to prevent relapse during this crucial time. This population would benefit from a screening tool that assesses for high-risk events like PTSD, psychological stress, and substance use triggers and intervention that includes evidence-based mental health resources.
References
The Organisation for Economic Co-operation and Development. Health status - Infant mortality rates - OECD Data. 2023. Available from: https://data.oecd.org/healthstat/infant-mortality-rates.htm. Last updated 2022; cited Sep 12, 2022.
Matoba N, Collins JW. Racial disparity in infant mortality. Semin Perinatol. 2017;41(6):354–9.
Brogly SB, Saia KE, Werler MM, Regan E, Hernández-Díaz S. Prenatal Treatment and Outcomes of Women With Opioid Use Disorder. Obstet Gynecol. 2018;132(4):916–22.
Daley DC. Family and social aspects of substance use disorders and treatment. J Food Drug Anal. 2013;21(4):S73–6.
Sanjuan PM, Pearson MR, Fokas K, Leeman LM. Supplemental Material for A Mother’s Bond: An Ecological Momentary Assessment Study of Posttraumatic Stress Disorder Symptoms and Substance Craving During Pregnancy. Psychol Addict Behav. 2019;34(2).
Schempf AH, Strobino DM. Illicit Drug Use and Adverse Birth Outcomes: Is It Drugs or Context? J Urban Health. 2008;85(6):858–73.
Kline-Simon AH, Chi FW, Mertens JR, Weisner C. Trajectories of remission and mortality over 13 years after intake to substance use treatment. Am J Drug Alcohol Abuse. 2017;43(5):583–90.
National Institute on Alcohol Abuse and Alcoholism. Recovery Research Definitions. Available from: https://www.niaaa.nih.gov/research/niaaa-recovery-from-alcohol-use-disorder/definitions. Cited Dec 09, 2022.
Madras BK, Compton WM, Avula D, Stegbauer T, Stein JB, Clark H Westley. Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: Comparison at intake and 6 months later. Drug Alcohol Depend. 2009;99(1-3):280–95.
Hargraves D, White C, Frederick R, Cinibulk M, Peters M, Young A, et al. Implementing SBIRT (Screening, Brief Intervention and Referral to Treatment) in primary care: lessons learned from a multi-practice evaluation portfolio. Public Health Rev. 2017;38(1).
Travers CP, Iannuzzi LA, Wingate MS, Avery DM, Ambalavanan N, Leeper J, et al. Prematurity and race account for much of the interstate variation in infant mortality rates in the United States. J Perinatol. 2020;40(5):767–73.
Trost SL, Beauregard JL, Smoots AN, Ko JY, Haight SC, Moore Simas TA, et al. Preventing Pregnancy-Related Mental Health Deaths: Insights From 14 US Maternal Mortality Review Committees, 2008–17. Health Aff. 2021;40(10):1551–9.
Walsh K, McCormack CA, Webster R, Pinto A, Lee S, Feng T, et al. Maternal prenatal stress phenotypes associate with fetal neurodevelopment and birth outcomes. Proc Natl Acad Sci U S A. 2019;116(48):23996–4005.
Dunkel Schetter C, Tanner L. Anxiety, depression and stress in pregnancy. Curr Opin Psychiatry. 2012;25(2):141–8.
Tyson DP, Kelleher KJ, Chavez LJ. Mental Health-related Utilization of Emergency Departments During Pregnancy in the U.S., 2016–2019. Matern Child Health J. 2022;26(10):1953–8.
Burris HH, Hacker MR. Birth outcome racial disparities: A result of intersecting social and environmental factors. Semin Perinatol. 2017;41(6):360–6.
Lorenz JM, Ananth CV, Polin RA, D’Alton ME. Infant mortality in the United States. J Perinatol. 2016;36(10):797–801.
Blumenshine P, Egerter S, Barclay CJ, Cubbin C, Braveman PA. Socioeconomic Disparities in Adverse Birth Outcomes. Am J Prev Med. 2010;39(3):263–72.
Fishman SH, Hummer RA, Sierra G, Hargrove T, Powers DA, Rogers RG. Race/ethnicity, maternal educational attainment, and infant mortality in the United States. Biodemography Soc Biol. 2020;66(1):1–26.
Office of the Surgeon General for United States Department of Health and Human Services. Addiction and Substance Misuse Reports and Publications. Available from: https://www.hhs.gov/surgeongeneral/reports-and-publications/addiction-and-substance-misuse/index.html. Last updated Mar 29, 2019; cited Dec 09, 2022.
Lewis B, Hoffman L, Garcia CC, Nixon SJ. Race and Socioeconomic Status in Substance Use Progression and Treatment Entry. J Ethn Subst Abuse. 2018;17(2):150–66.
Saloner B, Cook BL. Blacks And Hispanics Are Less Likely Than Whites To Complete Addiction Treatment, Largely Due To Socioeconomic Factors. Health Aff. 2013;32(1):135–45.
National Survey on Drug Use and Health. Key Substance Use and Mental Health Indicators in the United States: Results from the 2020 National Survey on Drug Use and Health. Available from: https://www.samhsa.gov/data/sites/default/files/reports/rpt35325/NSDUHFFRPDFWHTMLFiles2020/2020NSDUHFFR1PDFW102121.pdf. Last updated 2021; cited Dec 09, 2022.
Forray A, Yonkers KA. The Collision of Mental Health, Substance Use Disorder, and Suicide. Obstet Gynecol. 2021;137(6):1083-1090. Epub May 06, 2021.
National Institute on Drug Abuse. Substance Use in Women Drug Facts. Available from: https://nida.nih.gov/publications/drugfacts/substance-use-in-women. Last updated 2020; cited Dec 09, 2022.
Martin CE, Parlier-Ahmad AB. Addiction treatment in the postpartum period: an opportunity for evidence-based personalized medicine. Int Rev Psychiatry. 2021;33(6):579–90.
Walton-Moss BJ, McIntosh LC, Conrad J, Kiefer E. Health Status and Birth Outcomes Among Pregnant Women in Substance Abuse Treatment. Womens Health Issues. 2009;19(3):167–75.
Schiff DM, Nielsen T, Terplan M, Hood M, Bernson D, Diop H, et al. Fatal and Nonfatal Overdose Among Pregnant and Postpartum Women in Massachusetts. Obstet Gynecol. 2018;132(2):466–74.
Havens JR, Simmons LA, Shannon LM, Hansen WF. Factors associated with substance use during pregnancy: Results from a national sample. Drug Alcohol Depend. 2009; 99(1-3):89–95.
Terplan M, McNamara EJ, Chisolm MS. Pregnant and Non-Pregnant Women with Substance Use Disorders: The Gap Between Treatment Need and Receipt. J Addict Dis. 2012; 31(4):342–9.
Zedler BK, Mann AL, Kim MM, Amick HR, Joyce AR, Murrelle EL, et al. Buprenorphine compared with methadone to treat pregnant women with opioid use disorder: a systematic review and meta-analysis of safety in the mother, fetus and child. Addiction. 2016;111(12):2115–28.
Flavin J, Paltrow LM. Punishing pregnant drug-using women: Defying law, medicine, and common sense. J Addict Dis. 2010;29(2), 231–244.
Kelley AT, Smid MC, Baylis JD, Charron E, Begaye LJ, Binns-Calvey A, et al. Treatment access for opioid use disorder in pregnancy among rural and American Indian communities. J Subst Abuse Treat. 2021;136:108685.
Joshi C, Skeer MR, Chui K, Neupane G, Koirala R, Stopka TJ. Women-centered drug treatment models for pregnant women with opioid use disorder: A scoping review. Drug Alcohol Depend. 2021;226:108855.
Miele K, Kim SY, Jones R, Rembert J, Wachman E, Shrestha H. Medication for Opioid Use Disorder During Pregnancy — Maternal and Infant Network to Understand Outcomes Associated with Use of Medication for Opioid Use Disorder During Pregnancy (MAT-LINK), 2014–2021. MMWR Surveill Summ. 2023;72(No. SS-3):1-14.
Rosenthal EW, Short VL, Cruz Y, Barber C, Baxter JK, Abatemarco DJ, et al. Racial inequity in methadone dose at delivery in pregnant women with opioid use disorder. J Subst Abuse Treat. 2021;131:108454.
Knittel AK, Swartzwelder RA, Zarnick S, Tsujimoto THM, Horne T, Lin FC, et al. Medications for opioid use disorder during pregnancy: Access and continuity in a state women’s prison facility, 2016–2019. Drug Alcohol Depend. 2022;232:109308.
Suntai Z. Substance use among women who are pregnant: Examining treatment completion by race and ethnicity. J Subst Abuse Treat. 2021;131:108437.
Comfort M, Kaltenbach KA. Biopsychosocial Characteristics and Treatment Outcomes of Pregnant Cocaine-Dependent Women in Residential and Outpatient Substance Abuse Treatment. J Psychoact Drugs. 1999;31(3):279–89.
Buczkowski A, Avidan O, Cox D, Craig A. The Parental Experience of Newborns With Neonatal Abstinence Syndrome Across Inpatient Care Settings. J Addict Med. 2020;14(5):1.
Forray A, Merry B, Lin H, Ruger JP, Yonkers KA. Perinatal substance use: A prospective evaluation of abstinence and relapse. Drug Alcohol Depend. 2015;150:147–55.
McCarron H, Griese ER, Dippel E, McMahon TR. Cultural and Social Predictors of Substance Abuse Recovery among American Indian and Non-American Indian Pregnant and Parenting Women. J Psychoact Drugs. 2018;50(4):322–30.
Verissimo ADO, Grella CE. Influence of gender and race/ethnicity on perceived barriers to help-seeking for alcohol or drug problems. J Subst Abuse Treat. 2017;75:54–61.
Kelly JF, Greene MC, Bergman BG. Beyond Abstinence: Changes in Indices of Quality of Life with Time in Recovery in a Nationally Representative Sample of U.S. Adults. Alcohol Clin Exp Res. 2018;42(4):770–80.
Cunningham SD, Lewis JB, Shebl FM, Boyd LM, Robinson MA, Grilo SA, et al. Group Prenatal Care Reduces Risk of Preterm Birth and Low Birth Weight: A Matched Cohort Study. J Women’s Health. 2019;28(1):17–22.
Witte T, Amick M, Smith J. Recovery Identity and Psychosocial-Spiritual Health: A Survey of Individuals in Remission From Substance Use Disorders. J Drug Issues. 2022;53(3):002204262211330.
Schmidt CN, Wingo EE, Newmann SJ, Borne DE, Shapiro BJ, Seidman DL. Patient and provider perspectives on barriers and facilitators to reproductive healthcare access for women experiencing homelessness with substance use disorders in San Francisco. Women’s Health (London). 2023;19:174550572311523.
Stone R. Pregnant women and substance use: fear, stigma, and barriers to care. Health Justice. 2015;3(1).
Vrana C, Killeen T, Brant V, Mastrogiovanni J, Baker NL. Rationale, design, and implementation of a clinical trial of a mindfulness-based relapse prevention protocol for the treatment of women with comorbid post traumatic stress disorder and substance use disorder. Contemp Clin Trials. 2017;61:108–14.
Fallin-Bennett A, Elswick A, Ashford K. Peer support specialists and perinatal opioid use disorder: Someone that’s been there, lived it, seen it. Addict Behav. 2020;102:106204.
Asta D, Davis A, Krishnamurti T, Klocke L, Abdullah W, Krans EE. The influence of social relationships on substance use behaviors among pregnant women with opioid use disorder. Drug Alcohol Depend. 2021;222:108665.
Osterman R, Lewis D, Winhusen T. Efficacy of motivational enhancement therapy to decrease alcohol and illicit-drug use in pregnant substance users reporting baseline alcohol use. J Subst Abuse Treat. 2017;77:150–5.
Najavits LM, Weiss RD, Shaw SR, Muenz LR. “Seeking safety”: Outcome of a new cognitive-behavioral psychotherapy for women with posttraumatic stress disorder and substance dependence. J Trauma Stress. 1998;11(3):437–56.
Yonkers KA, Forray A, Howell HB, Gotman N, Kershaw T, Rounsaville BJ, et al. Motivational enhancement therapy coupled with cognitive behavioral therapy versus brief advice: a randomized trial for treatment of hazardous substance use in pregnancy and after delivery. Gen Hosp Psychiatry. 2012;34(5):439–49.
Xu X, Yonkers KA, Ruger JP. Costs of a Motivational Enhancement Therapy Coupled with Cognitive Behavioral Therapy versus Brief Advice for Pregnant Substance Users. PLoS One. 2014;9(4):e95264.
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Alexandra R. Dailey

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org







