Antibiotic Use Awareness and Practices in the Indian Community During Later Stages of COVID-19 Pandemic: A Cross-Sectional Survey
DOI:
https://doi.org/10.5195/ijms.2024.1885Keywords:
Drug Resistance, Microbial, Antimicrobial stewardship, Health knowledge, Attitudes, Practices, COVID 19, Antibiotic Use, Awareness, Indian Community, Antibiotic Resistance, Overuse, Self-Medication, Azithromycin, Regulations, Healthcare Professionals, Public Health, Infection, Stewardship Programs, Rational UseAbstract
Background: An increased overuse of antibiotics coupled with dearth of newer alternatives has worsened antibiotic resistance in LMIC’s like India. The prescription of antibiotics for symptoms similar to COVID-19 infection has aggravated the problem of antibiotic overuse, further worsening antibiotic resistance. This study aims at understanding not only the extent of overuse, but also the social patterns and causes of over-prescription or self medication of antibiotics in India.
Methods: A cross-sectional survey of the knowledge, attitude and practices on antibiotic use was conducted from September to October, 2022, using a Google form questionnaire. A virtual snowball technique was used to recruit respondents.
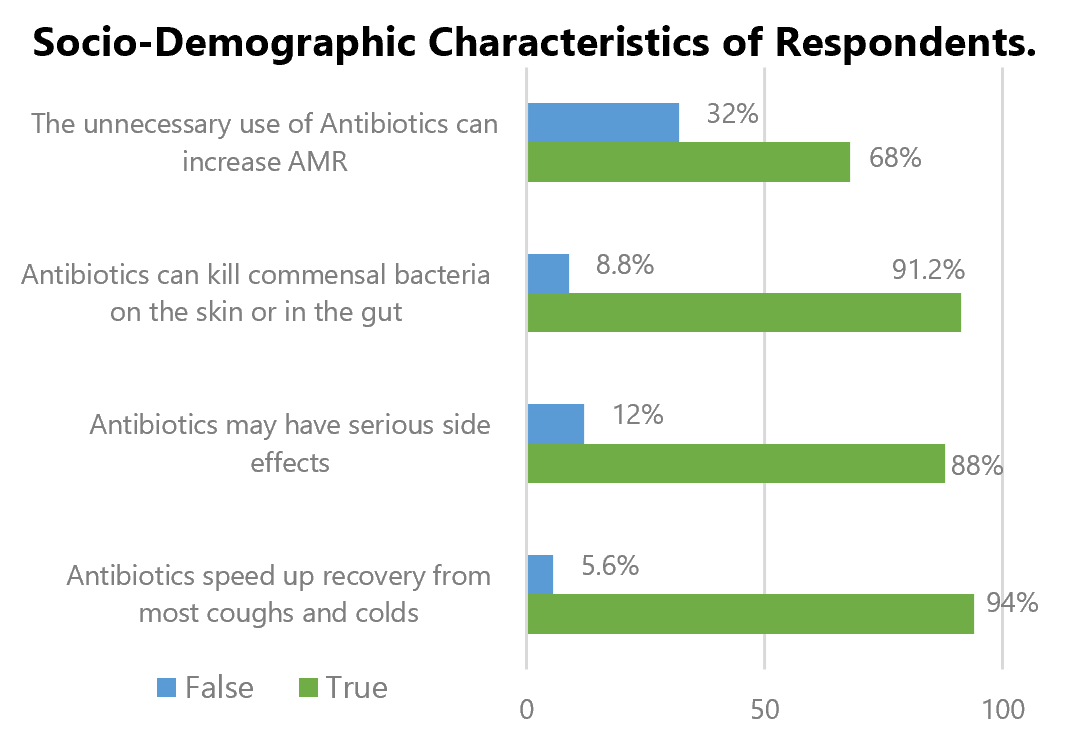
Results: A total of 309 responses were received (56% female and 44% male). 59.5% of the respondents were between 15 to 30 years. Surprisingly, in spite of a majority of respondents (around 70%) having a health sciences background, 67.8% of respondents falsely believe that antibiotics speed up recovery from most coughs and colds. 94.8% of respondents had used antibiotics in the last one year. 17.2% of respondents had taken antibiotics without the prescription of a doctor. The most common antibiotic used on prescription and self-medication was Azithromycin. Only 20.7% of respondents took antibiotics on suspicion of having COVID-19, with the most common one being Azithromycin.
Conclusion: The study highlights that a greater knowledge on antibiotic use does not necessitate better attitude towards their cautious and rational use. The use of antibiotics for self-limiting indications like cough, cold and sore throat needs to be restricted through stricter regulations.
References
Abat C, Gautret P, Raoult D. Benefits of antibiotics burden in low-income countries. Proc Natl Acad Sci USA.2018;115(35):E8109-E8110. DOI: https://doi.org/10.1073/pnas.1809354115
Klein EY, Van Boeckel TP, Martinez EM, Pant S, Gandra S, Levin SA et al. Global increase and geographic convergence in antibiotic consumption between 2000 and 2015. Proc Natl Acad Sci USA. 2018; 115(15):E3463-E3470. DOI: https://doi.org/10.1073/pnas.1717295115
Shallcross LJ, Davies DS. Antibiotic overuse: a key driver of antibiotic resistance. Br J Gen Pract.2014;64(629):604-5. DOI: https://doi.org/10.3399/bjgp14X682561
World Health Organization. Antibiotic resistance. Available from: https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance. Last Updated: 2021 17 Nov. Cited: 2022 23 Sept.
World Health Organization. Antibiotic resistance: global report on surveillance. Available from: https://apps.who.int/iris/handle/10665/112642. Last Updated: 2014. Cited: 2022 23 Sept.
Antibiotic Resistance Collaborators. Global burden of bacterial antibiotic resistance in 2019: a systematic analysis. Lancet. 2022; 399(10325):629-655. DOI: https://doi.org/10.1016/S0140-6736(21)02724-0
Liu Q, Jing W, Liu M, Liu J. Health disparity and mortality trends of infectious diseases in BRICS from 1990 to 2019. J Glob Health. 2022; 12:04028. DOI: https://doi.org/10.7189/jogh.12.04028
Klein EY, Tseng KK, Pant S, Laxminarayan R. Tracking global trends in the effectiveness of antibiotic therapy using the Drug Resistance Index. BMJ Glob Health. 2019; 4(2):e00 DOI: https://doi.org/10.1136/bmjgh-2018-001315
Sulis G, Batomen B, Kotwani A, Pai M, Gandra S. Sales of antibiotics and hydroxychloroquine in India during the COVID-19 epidemic: An interrupted time series analysis. PLoS Med. 2021; 18(7):e1003682. DOI: https://doi.org/10.1371/journal.pmed.1003682
Kotwani A, Joshi J, Lamkang AS. Over-the-Counter Sale of Antibiotics in India: A Qualitative Study of Providers' Perspectives across Two States. Antibiotics (Basel). 2021; 10(9):1123. DOI: https://doi.org/10.3390/antibiotics10091123
Indian Council of Medical Research (ICMR). Antibiotic Stewardship Program Guidelines. Available from: https://main.icmr.nic.in/sites/default/files/guidelines/AMSP_0.pdf. Cited: 2022 24 Sept.
World Health Organization. Clinical management of COVID-19. Available from: https://apps.who.int/iris/bitstream/handle/10665/332196/WHO-2019-nCoV-clinical-2020.5-eng.pdf. Last Updated: 2020 27 May. Cited: 2022 24 Sept
Hamers RL, van Doorn HR. Antibiotic consumption in low-income and middle-income countries. Lancet Glob Health. 2018; 6(7):e732. DOI: https://doi.org/10.1016/S2214-109X(18)30270-5
Awad AI, Aboud EA. Knowledge, attitude and practice towards antibiotic use among the public in Kuwait. PLoS One. 2015; 10(2):e0117910. DOI: https://doi.org/10.1371/journal.pone.0117910
Russom M, Bahta M, Debesai M, Bahta I, Kessete A, Afendi A et al. Knowledge, attitude and practice of antibiotics and their determinants in Eritrea: an urban population-based survey. BMJ Open. 2021; 11(9):e046432. DOI: https://doi.org/10.1136/bmjopen-2020-046432
Bhardwaj K, Shenoy S, Baliga S, Unnikrishnan B, Baliga BS. Knowledge, attitude, and practices related to antibiotic use and resistance among the general public of coastal south Karnataka, India–A cross-sectional survey Clin Epidem and Glob Hlth. 2021;11:100717. DOI: https://doi.org/10.1016/j.cegh.2021.100717
Alkhalifah HM, Alkhalifah KM, Alharthi AF, Elzahrany YR, Aljuhani MA. Knowledge, attitude and practices towards antibiotic use among patients attending Al Wazarat health center. J Family Med Prim Care. 2022; 11(4):1299-1307. DOI: https://doi.org/10.4103/jfmpc.jfmpc_1431_21
Akhtar Z, Mah-E-Muneer S, Rashid MM, Ahmed MS, Islam MA, Chowdhury S, et al. Antibiotics Use and Its Knowledge in the Community: A Mobile Phone Survey during the COVID-19 Pandemic in Bangladesh. Antibiotics 2021, 10, 1052. DOI: https://doi.org/10.3390/antibiotics10091052
André M, Vernby A, Berg J, Lundborg CS. A survey of public knowledge and awareness related to antibiotic use and resistance in Sweden. J Antimicrob Chemother. 2010; 65(6):1292-6. DOI: https://doi.org/10.1093/jac/dkq104
Napolitano F, Izzo MT, Di Giuseppe G, Angelillo IF. Public knowledge, attitudes, and experience regarding the use of antibiotics in Italy. PLoS One2013; 8(12):e84177. DOI: https://doi.org/10.1371/journal.pone.0084177
Peng D, Wang X, Xu Y, Sun C, Zhou X. Antibiotic misuse among university students in developed and less developed regions of China: a cross-sectional survey, Glob Health Action. 2018;11:1, 1496973. DOI: https://doi.org/10.1080/16549716.2018.1496973
Gupta MK, Vohra C, Raghav P. Assessment of knowledge, attitudes, and practices about antibiotic resistance among medical students in India. J Family Med Prim Care. 2019; 8(9):2864-2869. DOI: https://doi.org/10.4103/jfmpc.jfmpc_504_19
Nguyen LS, Dolladille C, Drici MD, Fenioux C, Alexandre J, Mira JP et al. Cardiovascular Toxicities Associated With Hydroxychloroquine and Azithromycin: An Analysis of the World Health Organization Pharmacovigilance Database. Circulation. 2020; 142(3):303-305. DOI: https://doi.org/10.1161/CIRCULATIONAHA.120.048238
Langford BJ, So M, Raybardhan S, Leung V, Soucy JR, Westwood D et al. Antibiotic prescribing in patients with COVID-19: rapid review and meta-analysis. Clin Microbiol Infect. 2021; 27(4):520-531. DOI: https://doi.org/10.1016/j.cmi.2020.12.018
Cho HJ, Hong SJ, Park S. Knowledge and beliefs of primary care physicians, pharmacists, and parents on antibiotic use for the pediatric common cold. Soc Sci Med. 2004; 58(3):623-9. DOI: https://doi.org/10.1016/S0277-9536(03)00231-4
World Health Organization. WHO AWaRe Antibiotic categorization. Available from: https://aware.essentialmeds.org/list. Last updated: 2019. Cited: 2022 27 Oct.
Khelgi A, Huchchannavar R, Mathew MM, Anandam S. Knowledge, attitude and practice regarding antibiotic use and antibiotic resistance among the rural public in Mangaluru, India. J Prev Epidemiol. 2022; 7(2):e26162. DOI: https://doi.org/10.34172/jpe.2022.26162
Yunita SL, Yang H-W, Chen Y-C, Kao L-T, Lu Y-Z, Wen Y-L et al. Knowledge and practices related to antibiotic use among women in Malang, Indonesia.Front. Pharmacol. 2022; 13:1019303. DOI: https://doi.org/10.3389/fphar.2022.1019303
Published
How to Cite
License
Copyright (c) 2024 Hiyanoor Ghosh, Dr. Kanchan Gupta

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org







