Continuous Rifampicin Therapy Induced Acute Kidney Injury in a Tuberculous Patient: A Case Report
DOI:
https://doi.org/10.5195/ijms.2024.1713Keywords:
Anti-tuberculosis, Rifampicin, Isoniazid, acute kidney injury, Tuberculosis.Abstract
Background: Tuberculosis (TB) presents with productive cough, hemoptysis, chest pain, fever, weight loss, and night sweats. Anti-tuberculosis treatment (ATT) can affect various organs, including the liver and kidneys. ATT-induced acute kidney injury (AKI) presents with fever, rash, nausea, vomiting, diarrhea, and abdominal pain. It occurs due to type 2 or 3 hypersensitivity and affects individuals who have previously used rifampicin or are currently using it intermittently.
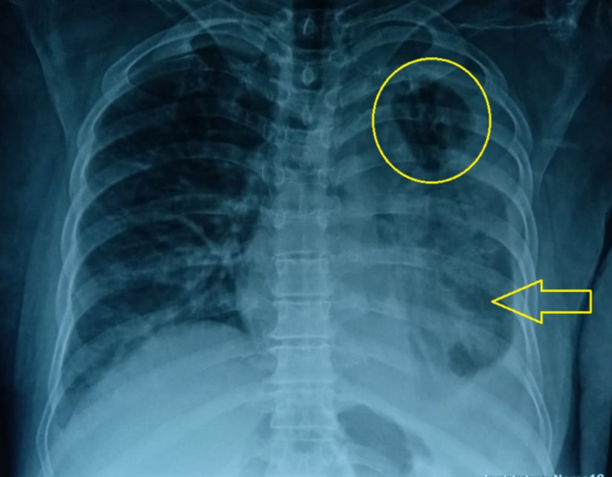
Case: An 60-year-old lady was diagnosed with TB and started on ATT. After a few days, she complained of reduced food intake and vomiting, yellow discoloration of the skin, abdominal pain and distention, and limb swelling. She was diagnosed as a case of ATT-induced AKI. She didn't have past exposure to rifampicin and was continuously using it this time.
Conclusion: The key learning point from this case is that ATT-induced AKI can develop even when used in a continuous dosing regime and upon first time exposure despite no history of past exposure. This prompts vigilance in monitoring renal function in patients being started on ATT regimen. This is becasuse, ATT-induced AKI poses risk to patient’s life and there is a possibility of developing resistance to anti-tuberculous therapy as a result of discontinuation of treatment. Furthermore, our case suggests that, in addition to immune-mediated mechanisms described in literature for ATT-induced AKI, other pathophysiological mechanisms might also be linked to this pathology and need further research for better understanding and optimization of treatment strategies.
References
1. Jeong YJ, Lee KS. Pulmonary tuberculosis: up-to-date imaging and management. AJR Am J Roentgenol. 2008;191(3):834–44. DOI: https://doi.org/10.2214/AJR.07.3896
World Health Organization. Tuberculosis (TB). Available from: https://www.who.int/news-room/fact-sheets/detail/tuberculosis. Last updated Nov 7, 2023; cited Feb 07, 2023.
Sakashita K, Murata K, Takahashi Y, Yamamoto M, Oohashi K, Sato Y, et al. A case series of acute kidney injury during anti-tuberculosis treatment. Intern Med. 2019;58(4):521–7. DOI: https://doi.org/10.2169/internalmedicine.0813-18
Chogtu B, Surendra VU, Magazine R, Acharya PR, Yerrapragada DB. Rifampicin-induced concomitant renal injury and hepatitis. J Clin Dian Res. 2016;10(9):0D18–9. DOI: https://doi.org/10.7860/JCDR/2016/21030.8578
Covic A, Goldsmith DJA, Segall L, Stoicescu C, Lungu S, Volovat C, et al. Rifampicin-induced acute renal failure: A series of 60 patients. Nephrol Dial Transplant. 1998;13(4):924–9. DOI: https://doi.org/10.1093/ndt/13.4.924
Shang P, Xia Y, Liu F, Wang X, Yuan Y, Hu D, et al. Incidence, clinical features and impact on anti-tuberculosis treatment of anti-tuberculosis drug induced liver injury (ATLI) in China. PLoS One. 2011;6(7):e21836. DOI: https://doi.org/10.1371/journal.pone.0021836
Tsang JY, Murray J, Kingdon E, Tomson C, Hallas K, Campbell S, et al. Guidance for post-discharge care following acute kidney injury: an appropriateness ratings evaluation. BJGP Open. 2020;4(3):bjgpopen20X101054. DOI: https://doi.org/10.3399/bjgpopen20X101054
Beebe A, Seaworth B, Patil N. Rifampicin-induced nephrotoxicity in a tuberculosis patient. J Clin Tuberc Other Mycobact Dis. 2015;1:13–5. DOI: https://doi.org/10.1016/j.jctube.2015.09.001
Schubert C, Bates WD, Moosa MR. Acute tubulointerstitial nephritis related to antituberculous drug therapy. Clin Nephrol. 2010;73(6):413–9. DOI: https://doi.org/10.5414/CNP73413
Chiba S, Tsuchiya K, Sakashita H, Ito E, Inase N. Rifampicin-induced acute kidney injury during the initial treatment for pulmonary tuberculosis: A case report and literature review. Intern Med. 2013;52(21):2457–60. DOI: https://doi.org/10.2169/internalmedicine.52.0634
Muthukumar T, Jayakumar M, Fernando EM, Muthusethupathi MA. Acute renal failure due to rifampicin: a study of 25 patients. Am J Kidney Dis. 2002;40(4):690–6. DOI: https://doi.org/10.1053/ajkd.2002.35675
De Vriese AS, Robbrecht DL, Vanholder RC, Vogelaers DP, Lameire NH. Rifampicin-associated acute renal failure: Pathophysiologic, immunologic, and clinical features. Am J Kidney Dis. 1998;31(1):108–15. DOI: https://doi.org/10.1053/ajkd.1998.v31.pm9428460
Smith EL, Bywater L, Pellicano R, Jenkin GA, Korman TM. Acute Tubular Necrosis and Thrombocytopenia Associated with Rifampin Use: Case Report and Review. Open Forum Infect Dis. 2022;9(7). DOI: https://doi.org/10.1093/ofid/ofac258
Ata F, Magboul HMB, Toba HAA, Alfar H, Al Bozom A, Murshed K, et al. Rifampin‐induced acute kidney injury and hemolysis: A case report and literature review of a rare condition. Clin Case Rep. 2022;10(12):e6780. DOI: https://doi.org/10.1002/ccr3.6780
Penn Medicine. Acute Kidney Injury (AKI) - Symptoms and Causes. Available from: https://www.pennmedicine.org/for-patients-and-visitors/patient-information/conditions-treated-a-to-z/acute-kidney-injury. Last updated Nov 4, 2022; cited Sep 14, 2022.
Chang CH, Chen YF, Wu VC, Shu CC, Lee CH, Wang JY, et al. Acute kidney injury due to anti-tuberculosis drugs: a five-year experience in an aging population. BMC Infect Dis. 2014;14(1):23. DOI: https://doi.org/10.1186/1471-2334-14-23
Sharma AP, Sural S, Gupta A, Garg AX, Gulati S, Sharma RK. Effect of antitubercular medications on blood pressure control in chronic kidney disease patients with tuberculosis: a prospective cohort study. J Nephrol. 2006;19(6):771–7.
Arem R. Hypoglycemia associated with renal failure. Endocrinol Metab Clin North Am. 1989;18(1):103–21. DOI: https://doi.org/10.1016/S0889-8529(18)30391-8
Fiaccadori E, Sabatino A, Morabito S, Bozzoli L, Donadio C, Maggiore U, et al. Hyper/hypoglycemia and acute kidney injury in critically ill patients. Clin Nutr. 2016(2):317-21. DOI: https://doi.org/10.1016/j.clnu.2015.04.006
Beck Jr. LH, Salant DJ. Harrison’s Principles of Internal Medicine. 20th ed. New York: McGraw-Hill Education; 2018.
Moussa C, Esbaa S, Rouis H, Sellami N, Hajji M, Houcine Y, et al. Rifampicin‐induced acute tubulointerstitial nephritis during pulmonary tuberculosis treatment: A case report. Respirol Case Rep. 2023;11(8):e01190. DOI: https://doi.org/10.1002/rcr2.1190
Moledina DG, Parikh CR. Differentiating acute interstitial nephritis from acute tubular injury: a challenge for clinicians. Nephron. 2019;143(3):211-6. DOI: https://doi.org/10.1159/000501207
Clarkson MR, Giblin L, O’Connell FP, O’Kelly P, Walshe JJ, Conlon P, et al. Acute interstitial nephritis: clinical features and response to corticosteroid therapy. Nephrol Dial Transplant. 2004;19(11):2778–83. DOI: https://doi.org/10.1093/ndt/gfh485
Lopes JA, Jorge S. The RIFLE and AKIN classifications for acute kidney injury: a critical and comprehensive review. Clin Kidney J. 2013;6(1):8–14. DOI: https://doi.org/10.1093/ckj/sfs160
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2024 Muqsit Ali Shaukat, Muhammad Fahad Ali, Ahmed Irtaza, Shehroz Yar Khan, Shad Muhammad Khan , Sohail Babar

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org







