Global Impact of Burnout Syndrome in Medical Students During the COVID-19 Pandemic: A Systematic Review
DOI:
https://doi.org/10.5195/ijms.2025.2511Keywords:
Academic Burnout;, Professional Burnout, COVID-19, Mental Health, Risk factors, Education, Medical, Undergraduate, Physical Activity, Psychosocial Intervention, Education, Distance, Pandemics, Academic PerformanceAbstract
Background: The prevalence of burnout syndrome among medical students is a growing concern, warranting comprehensive exploration, particularly in the context of the COVID-19 pandemic. This review aims to elucidate the burnout phenomenon, considering its impact on medical students' mental health, physical well-being, and academic performance.
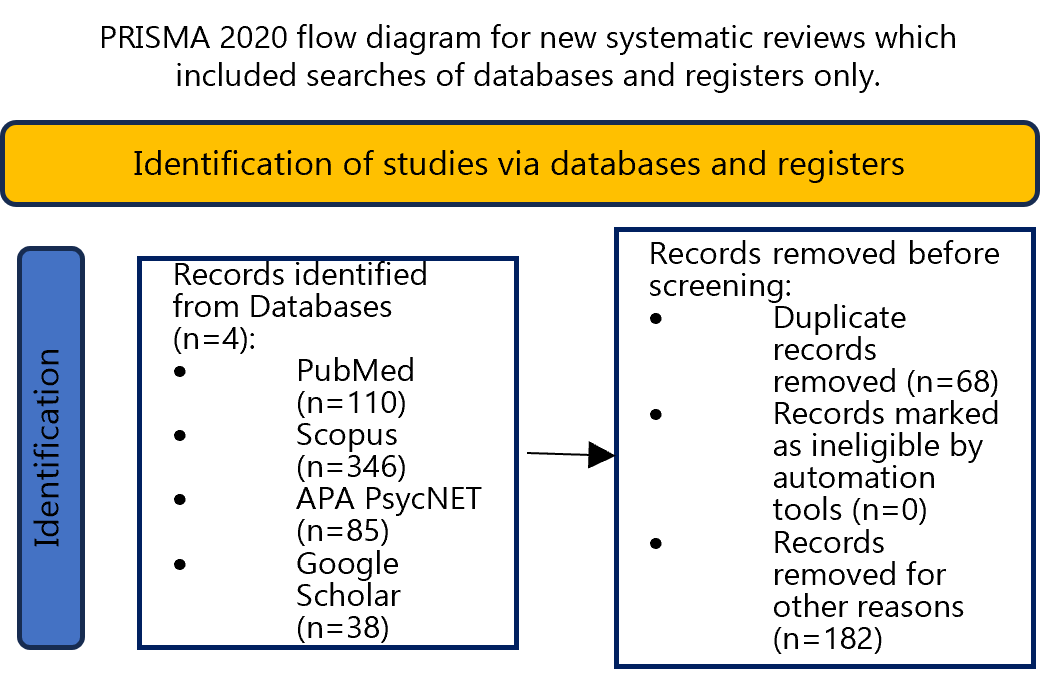
Methods: A thorough analysis was conducted, drawing on data from 31 studies encompassing over 37,000 participants in 25 countries. A systematic search across PubMed, Google Scholar, APA PsycNET, and Scopus utilized specific keyword combinations related to COVID-19, medical students, and burnout syndrome. The selected studies were evaluated to ensure relevance to the research aim.
Results: The review reveals burnout complexity, highlighting its diverse manifestations, exacerbated by the pandemic. Varied outcomes emerged from the studies, reflecting contrasting impacts on students. During lockdown, some reported having spent quality time with their families and delved into their academic interests, while others suffered due to the absence of clinical engagement. A notable correlation between burnout levels and academic year was observed, though interpretations differed among studies. Factors such as gender, family status, coping mechanisms, and the absence or presence of a supportive network were identified as influencers of burnout likelihood.
Conclusion: Medical student burnout persists as a significant challenge, intensified by pandemic disruptions to academic and clinical experiences. Urgent proactive measures by academic institutions are crucial to safeguard future physicians' well-being, with implications for enhancing healthcare delivery. This study underscores the immediate need to prioritize strategies for burnout prevention and management in medical education.
References
Aebischer O, Weilenmann S, Gachoud D, Méan M, Spiller TR. Physical and psychological health of medical students involved in the COVID-19 response in Switzerland. Swiss Med Wkly 2020;150:w20418.
Alkureishi ML, Jaishankar D, Dave S, Tatineni S, Zhu M, Chretien KC, et al. Impact of the early phase of the COVID-19 pandemic on medical student well-being: A multisite survey. J Gen Intern Med 2022;37:2156–64.
Almutairi H, Alsubaiei A, Abduljawad S, Alshatti A, Fekih-Romdhane F, Husni M, et al. Prevalence of burnout in medical students: A systematic review and meta-analysis. Int J Soc Psychiatry 2022;68:1157–70.
Asl EM, Boostani H, Behrouzian F, Rostami H. The mediating role of compassion in the relationship between COVID-19 anxiety syndrome and COVID-19 burnout. Journal of Education and Health Promotion 2021;10.
Bolatov AK, Seisembekov TZ, Askarova AZ, Baikanova RK, Smailova DS, Fabbro E. Online-learning due to COVID-19 improved mental health among medical students. Med Sci Educ 2021;31:183–92.
Bukhari GMJ, Saleem HB, Saleem J, Batool M, Majeed F, Batool H. The impact of covid-19 on the education of medical students of Federal Medical College, Islamabad, Pakistan. J Med Sci 2023;31.
WHO. Burn-out an “occupational phenomenon”: International Classification of Diseases. Available from: https://www.who.int/news/item/28-05-2019-burn-out-an-occupational-phenomenon-international-classification-of-diseases; updated 2019 May 28;
Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry 2016;15:103–11.
Campos R, Pinto V, Alves D, Rosa CP, Pereira H. Impact of COVID-19 on the mental health of medical students in Portugal. J Pers Med 2021;11:986.
Chunming WM, Harrison R, MacIntyre R, Travaglia J, Balasooriya C. Burnout in medical students: a systematic review of experiences in Chinese medical schools. BMC Med Educ 2017;17.
Compton S, Sarraf-Yazdi S, Rustandy F, Radha Krishna LK. Medical students’ preference for returning to the clinical setting during the COVID‐19 pandemic. Med Educ 2020;54:943–50.
Daryanto B, Kurniawan J, Wiranigitasari, Hioe F, Nurhadi P, Yudhantara DS. Prevalence of burnout and its associated factors among medical students during COVID-19 pandemic in Indonesia: A cross-sectional study. PLoS One 2023;18:e0285986.
de Andres Crespo M, Claireaux H, Handa AI. Medical students and COVID-19: lessons learnt from the 2020 pandemic. Postgrad Med J 2021;97:209–10.
Duarte I, Alves A, Coelho A, Ferreira A, Cabral B, Silva B, et al. The mediating role of resilience and life satisfaction in the relationship between stress and burnout in medical students during the COVID-19 pandemic. Int J Environ Res Public Health 2022;19:2822.
Ekmekci̇ Ertek İ, Özkan S, Candansayar S, İlhan M. The impact of the COVID-19 pandemic on the mental health of medical students. J Surg Med 2022;6:162–7. https://doi.org/10.28982/josam.1061178.
El Mouedden I, Hellemans C, Anthierens S, Michels NR, DeSmet A. Experiences of academic and professional burn-out in medical students and residents during first COVID-19 lockdown in Belgium: a mixed-method survey. BMC Med Educ 2022;22.
Ernst J, Jordan K-D, Weilenmann S, Sazpinar O, Gehrke S, Paolercio F, et al. Burnout, depression and anxiety among Swiss medical students – A network analysis. J Psychiatr Res 2021;143:196–201.
Esguerra S, Chiu FT, Espinoza A, Williams D, Clithero-Eridon A. Are medical students happy despite unhappy conditions: a qualitative exploration of medical student cohorts during disruptive conditions. BMC Med Educ 2023;23.
Forycka J, Pawłowicz-Szlarska E, Burczyńska A, Cegielska N, Harendarz K, Nowicki M. Polish medical students facing the pandemic—Assessment of resilience, well-being and burnout in the COVID-19 era. PLoS One 2022;17:e0261652.
Frajerman A, Chaumette B, Krebs M-O, Morvan Y. Mental health in medical, dental and pharmacy students: A cross-sectional study. J Affect Disord Rep 2022;10:100404. https://doi.org/10.1016/j.jadr.2022.100404.
Golui P, Roy S, Dey I, Burman J, Sembiah S. Resilience and its correlates among medical students in the Eastern part of India during the coronavirus disease 2019 (COVID-19) pandemic. J Family Community Med 2022;29.
Guadix SW, Sha C, Sandrone S, Safdieh JE, Sarva H. The impact of COVID-19 on neurology education: A medical student perspective. Front Educ 2020;5. https://doi.org/10.3389/feduc.2020.567421.
Halperin SJ, Henderson MN, Prenner S, Grauer JN. Prevalence of anxiety and depression among medical students during the Covid-19 pandemic: A cross-sectional study. J Med Educ Curric Dev 2021;8:238212052199115.
Hansell MW, Ungerleider RM, Brooks CA, Knudson MP, Kirk JK, Ungerleider JD. Temporal Trends in Medical Student Burnout. Fam Med 2019;51:399–404.
Harries AJ, Lee C, Jones L, Rodriguez RM, Davis JA, Boysen-Osborn M, et al. Effects of the COVID-19 pandemic on medical students: a multicenter quantitative study. BMC Med Educ 2021;21.
Ifrah Naaz S, Hussein RM, Khan HB, Hussein MM, Arain SA. Emotional responses and coping strategies of medical students during the COVID-19 pandemic. Saudi Med J 2022;43:61–6.
Ilić IM, Ilić MD. The relationship between the burnout syndrome and academic success of medical students: a cross-sectional study. Arh Hig Rada Toksikol 2023;74:134–41.
IsHak W, Nikravesh R, Lederer S, Perry R, Ogunyemi D, Bernstein C. Burnout in medical students: a systematic review. Clin Teach 2013;10:242–5.
Jezzini-Martinez S, Martinez-Garza JH, Quiroga-Garza A, Quiroz-Perales XG, Gil-Flores L, de la Fuente-Villarreal D, et al. Assessment of burnout syndrome and associated factors among medical students during the COVID-19 pandemic. J Affect Disord Rep 2023;14:100616.
Joshi VR, Younger JM, Das S, Goud BKM, Pramanik K. Factors influencing burnout in millennial medical students during the COVID-19 pandemic! Ir J Med Sci 2023;192:513–9.
Kalauni BR, Prasad Joshi Y, Paudel K, Aryal B, Karki L, Paudel R. Depression, anxiety and stress among undergraduate health sciences students during COVID-19 pandemic in a low resource setting: a cross sectional survey from Nepal. Ann Med Surg (Lond) 2023;Publish Ahead of Print.
Kasemy ZA, Sharif AF, Barakat AM, Abdelmohsen SR, Hassan NH, Hegazy NN, et al. Technostress creators and outcomes among Egyptian medical staff and students: A multicenter cross-sectional study of remote working environment during COVID-19 pandemic. Front Public Health 2022;10.
Liu Y, Cao Z. The impact of social support and stress on academic burnout among medical students in online learning: The mediating role of resilience. Front Public Health 2022;10.
Luberto CM, Goodman JH, Halvorson B, Wang A, Haramati A. Stress and coping among health professions students during COVID-19: A perspective on the benefits of mindfulness. Glob Adv Health Med 2020;9:216495612097782. .
Metakides C, Pielemeier L, Lytras T, Mytilinaios DG, Themistocleous SC, Pieridi C, et al. Burnout and motivation to study medicine among students during the COVID-19 pandemic. Front Med (Lausanne) 2023;10.
Minh LD, Phan HH, Le Mai DN, Dat NT, Tri NM, Ha NV, et al. Pattern and perceived changes in quality of life of Vietnamese medical and nursing students during the COVID-19 pandemic. PLoS One 2022;17:e0279446.
Muaddi MA, El-Setouhy M, Alharbi AA, Makeen AM, Adawi EA, Gohal G, et al. Assessment of medical students burnout during COVID-19 pandemic. Int J Environ Res Public Health 2023;20:3560.
Nakhostin-Ansari A, Akhlaghi M, Etesam F, Sadeghian MH. Suicidal ideation and its associated factors in medical, dental, and pharmacy students: A cross-sectional study during COVID-19 pandemic. Psychiatry J 2022;2022:1–10.
Nasr C, Bou Sanayeh E, Nasr C, Merheb G, Massoud M. Burnout rates among Lebanese pre-final and final year medical students during the COVID-19 pandemic: A multi-centered survey-based study. Work 2023;74:1265–76.
Natalia D, Syakurah RA. Mental health state in medical students during COVID-19 pandemic. Journal of Education and Health Promotion 2021;10.
Peng P, Hao Y, Liu Y, Chen S, Wang Y, Yang Q, et al. The prevalence and risk factors of mental problems in medical students during COVID-19 pandemic: A systematic review and meta-analysis. J Affect Disord 2023;321:167–81
Phillips HE, Jennings RB, Outhwaite IR, Grosser S, Chandra M, Ende V, et al. Motivation to impact: Medical student volunteerism in the COVID 19 pandemic. Med Sci Educ 2022;32:1149–57.
Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the conduct of narrative synthesis in systematic reviews A product from the ESRC methods programme. Lancaster.ac.uk 2006. https://www.lancaster.ac.uk/media/lancaster-university/content- assets/documents/fhm/dhr/chir/NSsynthesisguidanceVersion1-April2006.pdf
Qu R, Ding N, Li H, Song X, Cong Z, Cai R, et al. The mediating role of general academic emotions in burnout and procrastination among Chinese medical undergraduates during the COVID-19 pandemic: A cross-sectional study. Front Public Health 2022;10.
Rolland F, Hadouiri N, Haas-Jordache A, Gouy E, Mathieu L, Goulard A, et al. Mental health and working conditions among French medical students: A nationwide study. J Affect Disord 2022;306:124–30.
Ruiz R, Fernandes DA, Vásquez A, Trigueros A, Pemberton M, Gnanapragasam SN, et al. Prevalence of burnout in medical students in Guatemala: Before and during Covid-19 pandemic comparison. Int J Soc Psychiatry 2022;68:1213–7.
Saeki S, Shimato M. Mental health support for the current and future medical professionals during pandemics. JMA J 2021;4:281–3.
Shadid A, Shadid AM, Shadid A, Almutairi FE, Almotairi KE, Aldarwish T, et al. Stress, burnout, and associated risk factors in medical students. Cureus 2020.
Shpakou A, Naumau IA, Krestyaninova TY, Znatnova AV, Lollini SV, Surkov S, et al. Physical activity, life satisfaction, stress perception and coping strategies of university students in Belarus during the COVID-19 pandemic. Int J Environ Res Public Health 2022;19:8629. .
Silistraru I, Olariu O, Ciubara A, Roșca Ștefan, Roșca RO, Stanciu S, et al. Burnout and online medical education: Romanian students in lockdown and their residency choices. Int J Environ Res Public Health 2022;19:5449.
Šimić Š, Černy OE, Bevanda M, Bevanda D, Rizikalo A, Marijanović I. Impact of COVID-19 pandemic on mental health of medical students at the university of mostar. Psychiatr Danub 2021;33 (Suppl 10):114-119. PMID: 34672283.
Sulaiman R, Ismail S, Shraim M, El Hajj MS, Kane T, El-Awaisi A. Experiences of burnout, anxiety, and empathy among health profession students in Qatar University during the COVID-19 pandemic: a cross-sectional study. BMC Psychol 2023;11.
Tee KR, Ismail AS, Ang YH, Hishamuddin HH, Paul VJ, Aizuddin AN, et al. Prevalence of anxiety and burnout, and coping mechanisms among clinical year medical undergraduate students in Universiti Kebangsaan Malaysia amidst the COVID-19 pandemic. Int J Environ Res Public Health 2022;19:13010.
Tokumasu K, Nishimura Y, Sakamoto Y, Obika M, Kataoka H, Otsuka F. Differences in stress perception of medical students depending on in-person communication and online communication during the COVID−19 pandemic: A Japanese cross-sectional survey. Int J Environ Res Public Health 2023;20:1579.
Wercelens VO, Bueno ML, Bueno JL, Abrahim RP, Ydy JGM, Zanetti HR, et al. Empathy and psychological concerns among medical students in Brazil during the COVID-19 pandemic. Int J Psychiatry Med 2023;58:510–21. .
Wilkes TC, Lewis T, Paget M, Holm J, Brager N, Bulloch A, et al. Wellbeing and mental health amongst medical students in Canada. Int J Soc Psychiatry 2022;68:1283–8
Wissing RO, Hilverda F, Scheepers RA, Nieboer AP, Vollmann M. Peer relationships buffer the negative association of online education with education satisfaction and subsequently with study engagement among undergraduate medical students. BMC Med Educ 2022;22.
Yang Q, Liu Y, Yang WF, Peng P, Chen S, Wang Y, et al. Mental health conditions and academic burnout among medical and non-medical undergraduates during the mitigation of COVID-19 pandemic in China. Environ Sci Pollut Res Int 2022;29:57851–9.
Zhang J-Y, Shu T, Xiang M, Feng Z-C. Learning burnout: Evaluating the role of social support in medical students. Front Psychol 2021;12.
Zis P, Artemiadis A, Bargiotas P, Nteveros A, Hadjigeorgiou GM. Medical studies during the COVID-19 pandemic: The impact of digital learning on medical students’ burnout and mental health. Int J Environ Res Public Health 2021;18:349.
Žuljević MF, Jeličić K, Viđak M, Đogaš V, Buljan I. Impact of the first COVID-19 lockdown on study satisfaction and burnout in medical students in Split, Croatia: a cross-sectional presurvey and postsurvey. BMJ Open 2021;11:e049590.
Zúñiga D, Torres-Sahli M, Nitsche P, Echeverría G, Pedrals N, Grassi B, et al. Reduced burnout and higher mindfulness in medical students after a self-care program during the COVID-19 pandemic. Rev Med Chil 2021;149:846–55.
Sreeramareddy CT, Shankar PR, Binu VS, Mukhopadhyay C, Ray B, Menezes RG. Psychological morbidity, sources of stress and coping strategies among undergraduate medical students of Nepal. BMC Med Educ 2007;7.
CASP checklists. CASP - Critical Appraisal Skills Programme n.d. https://casp-uk.net/casp-toolschecklists/.
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2025 Maria Konstantina Tzioti, Athanasios Douzenis

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org







