A Case-Based Discussion Supporting Ethics Education in Medical Schools
DOI:
https://doi.org/10.5195/ijms.2023.2046Keywords:
Patient Self-Determination Act, Patient-centered healthcare, Advance directives, Incapacitated, unrepresented patients, Ethical awareness in healthcare providers, Ethics education in medical schools, Ethical literacy, Clinical ethics, Case-based discussion, Autonomy in medical decision-making, Capacity assessment, Vulnerability of homeless patients, Stigmatization of psychiatric illness, Ethics curriculum in medical education, Ethical dilemmas in patient care, Provider uncertainty, Patient autonomy, Standardized ethics education, Hands-on ethics training, Humanistic ethics in healthcareAbstract
Background: Ethics education in medical schools lacks uniformity, yielding uncertainty when providers are faced with ethically complex patients. Without streamlined ethics training, providers are less confident in their ability to provide ethically appropriate care for all patients, particularly for those most ethically vulnerable. This case report seeks to elucidate ethical concerns when treating an ethically complex patient. Subsequently, the need for early ethics education is substantiated.
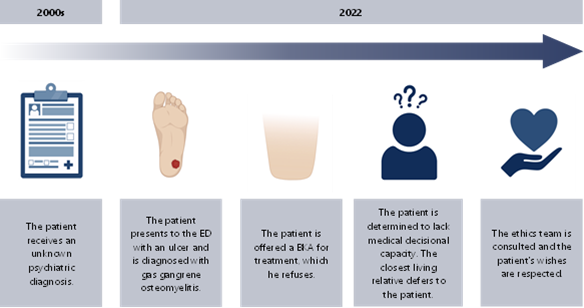
The Case: A 58-year-old unhoused patient with no known medical history presented to the emergency department (ED) for evaluation of an infected foot wound. Imaging confirmed acute gas gangrene osteomyelitis. The patient refused the recommended below-the-knee amputation (BKA) but was amenable to intravenous antibiotic therapy. He was subsequently determined by psychiatry to lack decisional capacity and met the DSM-5 criteria for schizoaffective psychosis. Subsequently, the patient’s brother deferred decision-making to the patient, who he believed should make his own medical decisions. Following an ethics consultation, the brother’s decision, and by proxy the patient’s, was respected.
Conclusion: In this case, the patient’s autonomy was prioritized, despite his high level of ethical vulnerability. Ethically conscious treatment was provided despite the implicit stigmatization of homelessness and psychiatric illness. However, an ethics consultation was necessary for this to occur. Ultimately, this paper should serve as a call to action for standardization and prioritization of ethics education during and beyond medical training.
References
Brown M. Who Would You Choose? Appointing an Agent with a Medical Power of Attorney. J Am Geriatr Soc. 1997;16(4):147–50. DOI: https://doi.org/10.1111/j.1741-6612.1997.tb01038.x
Pope T. Unbefriended And Unrepresented: Better Medical Decision Making For Incapacitated Patients Without Healthcare Surrogates. Georgia State University Law Review. 2017;
Pellegrino E, Siegler M, Singer P. Teaching clinical ethics. J Clin Ethics. 1990 Fall;1(3):175-80. DOI: https://doi.org/10.1086/JCE199001302
Appelbaum PS, Grisso T. Assessing Patients’ Capacities to Consent to Treatment. N Engl J Med. 1988;319(25):1635–8. DOI: https://doi.org/10.1056/NEJM198812223192504
Appel JM. A Values-Based Approach to Capacity Assessment. J Leg Med. 2022;42(1–2):53–65. DOI: https://doi.org/10.1080/01947648.2022.2162171
Curlin FA, Lawrence RE, Fredrickson J. An Ethical Façade? Medical Students’ Miscomprehensions of Substituted Judgment. Von Elm E, editor. PLoS ONE. 2009;4(2):e4374. DOI: https://doi.org/10.1371/journal.pone.0004374
Gilmer C, Buccieri K. Homeless Patients Associate Clinician Bias With Suboptimal Care for Mental Illness, Addictions, and Chronic Pain. J Prim Care Community Health. 2020;11:215013272091028. DOI: https://doi.org/10.1177/2150132720910289
Kisely S, Campbell LA, Wang Y. Treatment of ischaemic heart disease and stroke in individuals with psychosis under universal healthcare. Br J Psychiatry. 2009;195(6):545–50. DOI: https://doi.org/10.1192/bjp.bp.109.067082
Fakhoury WKH, White I, Priebe S. Be Good to Your Patient: How the Therapeutic Relationship in the Treatment of Patients Admitted to Assertive Outreach Affects Rehospitalization. J Nerv Ment Dis. 2007;195(9):789–91. DOI: https://doi.org/10.1097/NMD.0b013e318142cf5e
Culver CM, Clouser KD, Gert B, Brody H, Fletcher J, Jonsen A, et al. Basic Curricular Goals in Medical Ethics. N Engl J Med. 1985;312(4):253–6. DOI: https://doi.org/10.1056/NEJM198501243120430
DuBois JM, Burkemper J. Ethics Education in U.S. Medical Schools: A Study of Syllabi. Acad Med. 2002;77(5):432–7. DOI: https://doi.org/10.1097/00001888-200205000-00019
Beigy M, Pishgahi G, Moghaddas F, Maghbouli N, Shirbache K, Asghari F, et al. Students’ medical ethics rounds: a combinatorial program for medical ethics education. J Med Ethics Hist Med. 2016;9:3.
Published
How to Cite
Issue
Section
Categories
License
Copyright (c) 2023 Liliana Ladner, Mark G. Swope, Phyllis Whitehead

This work is licensed under a Creative Commons Attribution 4.0 International License.
Authors who publish with this journal agree to the following terms:
- The Author retains copyright in the Work, where the term “Work” shall include all digital objects that may result in subsequent electronic publication or distribution.
- Upon acceptance of the Work, the author shall grant to the Publisher the right of first publication of the Work.
- The Author shall grant to the Publisher and its agents the nonexclusive perpetual right and license to publish, archive, and make accessible the Work in whole or in part in all forms of media now or hereafter known under a Creative Commons Attribution 4.0 International License or its equivalent, which, for the avoidance of doubt, allows others to copy, distribute, and transmit the Work under the following conditions:
- Attribution—other users must attribute the Work in the manner specified by the author as indicated on the journal Web site; with the understanding that the above condition can be waived with permission from the Author and that where the Work or any of its elements is in the public domain under applicable law, that status is in no way affected by the license.
- The Author is able to enter into separate, additional contractual arrangements for the nonexclusive distribution of the journal's published version of the Work (e.g., post it to an institutional repository or publish it in a book), as long as there is provided in the document an acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post online a prepublication manuscript (but not the Publisher’s final formatted PDF version of the Work) in institutional repositories or on their Websites prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work. Any such posting made before acceptance and publication of the Work shall be updated upon publication to include a reference to the Publisher-assigned DOI (Digital Object Identifier) and a link to the online abstract for the final published Work in the Journal.
- Upon Publisher’s request, the Author agrees to furnish promptly to Publisher, at the Author’s own expense, written evidence of the permissions, licenses, and consents for use of third-party material included within the Work, except as determined by Publisher to be covered by the principles of Fair Use.
- The Author represents and warrants that:
- the Work is the Author’s original work;
- the Author has not transferred, and will not transfer, exclusive rights in the Work to any third party;
- the Work is not pending review or under consideration by another publisher;
- the Work has not previously been published;
- the Work contains no misrepresentation or infringement of the Work or property of other authors or third parties; and
- the Work contains no libel, invasion of privacy, or other unlawful matter.
- The Author agrees to indemnify and hold Publisher harmless from the Author’s breach of the representations and warranties contained in Paragraph 6 above, as well as any claim or proceeding relating to Publisher’s use and publication of any content contained in the Work, including third-party content.
Enforcement of copyright
The IJMS takes the protection of copyright very seriously.
If the IJMS discovers that you have used its copyright materials in contravention of the license above, the IJMS may bring legal proceedings against you seeking reparation and an injunction to stop you using those materials. You could also be ordered to pay legal costs.
If you become aware of any use of the IJMS' copyright materials that contravenes or may contravene the license above, please report this by email to contact@ijms.org
Infringing material
If you become aware of any material on the website that you believe infringes your or any other person's copyright, please report this by email to contact@ijms.org







